Healthcare shouldn't end when patients leave the doctor's office.
A dedicated care team that operates as an extension of your primary care provider — transforming outcomes one patient at a time.
Comprehensive Care Coordination
Personalized care plans built through real conversations about health needs and goals. Our service-first approach is backed by technology — focused entirely on the patient.
Chronic Care Management
Qualifying patients are contacted 2–3 times monthly by our care team. Our high-touch approach catches the little things before they become big issues.
Behavioral Health
Customized, high-quality psychiatric and psychological care from the comfort and convenience of the patient's home. Addressing depression, isolation, and more.
Care Coordination
Medication reconciliation, referral management, chart updates, appointment scheduling, and post-discharge follow-up — handled seamlessly as an extension of your practice.
Proactive Virtual Health
Direct patient engagement on a regular basis. We work hand-in-hand with patients to address their needs, deliver outcomes, and keep providers informed.
Full Medicare Reimbursement
Our services are 100% reimbursed by Medicare at zero cost to patients or providers. We handle all billing and administrative logistics.
Delivering Outcomes One Patient at a Time
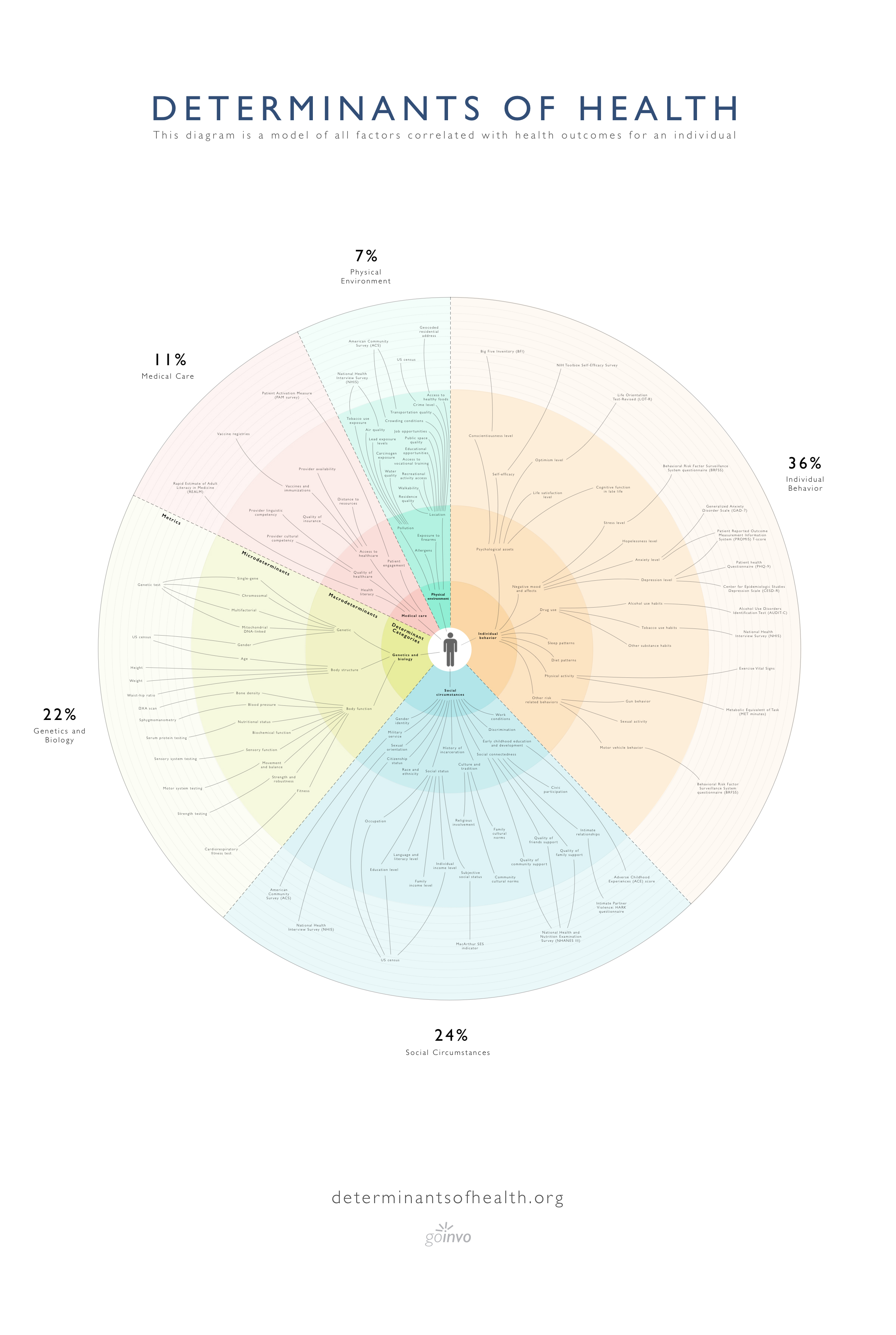
Healthcare in the US costs over $3.3 trillion — 18% of GDP — with more than 80% driven by chronic disease. Yet medical care only accounts for 10–20% of health outcomes. The rest depends on social, behavioral, and environmental factors.
That's where we come in. Continuity Care builds lasting relationships with patients through regular, meaningful conversations. We don't just track conditions — we address the whole person: nutrition, mental health, medication adherence, social needs, and more.
Our care plans are personalized for every patient, because healthcare is a personal journey and everyone is dealt a different hand in life. With high-touch, individualized attention, every patient develops a real relationship with their care manager.

How It Works
Enrollment
Your practice identifies eligible Medicare patients with two or more chronic conditions. We handle patient outreach and consent.
Personal Care Team
Each patient is assigned a dedicated care manager who builds a real relationship through regular phone check-ins — 2 to 3 times per month.
Ongoing Coordination
Monthly touch points, medication management, referrals, and proactive wellness support — all documented and shared with the provider.
Addressing Social Determinants of Health
Medical care alone accounts for only 10–20% of health outcomes. The rest — behavior, social circumstances, economic stability, and environment — are the social determinants of health (SDOH) that shape whether patients thrive or struggle.
This is especially critical in mission-driven organizations like FQHCs, where patients often face compounding barriers: food insecurity, housing instability, transportation challenges, and limited access to specialists. Traditional care models miss these factors entirely.
Continuity Care's model is built to close that gap. Through regular, meaningful conversations, our care managers identify SDOH barriers and connect patients with real solutions — because a care plan that ignores a patient's life outside the clinic isn't a care plan at all.
Housing & Stability
Connecting patients with rental assistance, Section 8, and community housing resources
Food & Nutrition
Nutrition coaching, food program referrals, and dietary planning for chronic conditions
Community & Social Services
Bilingual support, behavioral health referrals, transportation, and combating isolation
Patient Stories
Every patient has a story. Here's how continuity of care is making a difference.
Oscar has diabetes and smoked a pack of cigarettes a day since his teens. Since signing up with Continuity Care, his care manager checks in every week. He's now working on a plant-based eating plan and reduced smoking from a pack a day to one pack a week — regaining control over his health.Oscar — Diabetes & Lifestyle Management
I was on 5 different blood pressure meds and had recently been experiencing intermittent drops in my BP. Jeanette, my care manager, reassured me and escalated the issue to my doctors. My dosage was changed the very next day and I finally got my blood pressure under control.CCM Patient — Blood Pressure Management
My patient lost his house in Hurricane Harvey and was living with his daughter. Continuity Care's staff found a Section 8 rental assistance program, guided the patient through the process, and he was able to find a new place to live. That's addressing the whole person.Physician — Social Determinants of Health
Built for the Organizations That Need It Most
FQHCs and mission-driven practices serve the patients who face the greatest barriers to care — but often lack the administrative resources to deliver chronic care management at scale. We operate seamlessly as an extension of your care team, so you can focus on your mission.
- Purpose-built for FQHCs and safety-net providers
- White-labeled service — patients see your brand
- 100% Medicare reimbursed — sustainable revenue stream
- Achieve MIPS, MACRA, and UDS quality measures
- SDOH data collection and community resource coordination
- Bilingual care teams — Spanish and other languages
- Reduce hospital readmissions and ER visits
- No upfront costs or long-term contracts

Contact Us
We're committed to driving patient engagement in a sustainable and scalable manner. Whether you're a provider, an FQHC, or want to learn more about our services — we'd love to hear from you.



